Jun 28, 2016
By Sarbajit Mukherjee, MBBS
University of Oklahoma Health Sciences Center
“When human judgment and big data intersect, there are some funny things that happen.” —Nate Silver
Oncologists are deeply involved in the intersection of human judgement and data, which we typically just call “research.” However, when you’re trying to conduct research in an oncology training program, it may not seem exactly funny, and in fact can be quite challenging.
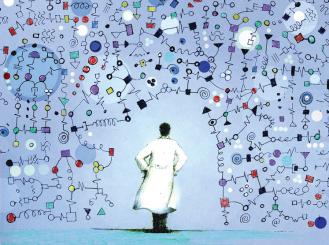
Oncology is one of the most academic disciplines of medicine, and its scientific concepts are rapidly evolving. Over the past few years, a convergence of innovations—whole-genome sequencing enabling us to interrogate each tumor individually, molecularly driven therapeutic developments, and revolutionary advancements in immunology— has created an unprecedented opportunity for us to make a big impact on cancer. Consequently, this has attracted a number of brilliant clinicians and scientists to this field.
Most oncology training programs around the nation are also integrated with hematology training to a combined 3-year hematology-oncology fellowship. The Accreditation Council for Graduate Medical Education (ACGME), an independent nonprofit organization, meticulously monitors the training programs throughout the United States to ensure excellence in medical education and quality patient care.
Participation in scholarly activities, which include research, evidence-based presentations at journal clubs or meetings, or preparation and submission of articles for peer-reviewed publications, is required by ACGME for fellows to graduate. Although research is not a mandatory requirement by ACGME, most academic institutions encourage their fellows to participate in some research activities during training.
Research can be extremely rewarding for fellows, as a successful project may lead to intellectual satisfaction, a sense of accomplishment, and useful contributions to our body of knowledge. Depending on the resources, mentorship, and time available for research, fellows may choose to participate in observational, clinical, translational, or basic science research. In addition, some training programs may offer intense research training to their fellows through additional degree courses (master’s, doctorate, etc.).
Some of the barriers to research during training have been identified through surveys that involved internal medicine training program directors and residents.1 Most of these issues are applicable to hematology-oncology fellowship as well. They include limited fellow time, difficulty finding a mentor, inadequate faculty time, and lack of funding.
In the recent era of electronic medical records, where extensive documentation requires a significant amount of physician’s time, pursuing research or other academic interests has become more challenging and often occurs at the cost of a physician investigator’s personal time. This could be even more pressing for fellows at the beginning of their careers due to competitive clinical responsibilities and a huge demand for learning at the same time. Many fellowship programs are frontloaded with clinical rotations, which leaves a limited amount of time for fellows to pursue and complete a project during their training.
Starting a project early is very important. Fellowship programs can assist by assigning their fellows’ research and clinical rotations in a way that fellows may identify and start working on a project early during their training. Setting a research curriculum and offering intense research mentoring programs have also been shown to promote scholarly activities, often leading to a successful academic career.2,3 Combining graduate coursework and research training with subspecialty fellowship is another way of training and retaining physicians in academic medicine.4
Although most academic institutions have clinicians and scientists working on a wide variety of topics, identifying a mentor with similar research interests can be a challenging job for a fellow. Even when a mentor is available, competing responsibilities of both the mentor and the fellow may make it difficult to spend adequate time on a project.
A successful mentorship requires active efforts from both the mentor and the mentee. A successful mentor should be altruistic, be an effective listener, provide honest feedback, and prioritize the mentee’s interests.5 On the other hand, a mentee should be responsible, respectful to their mentor(s), and attentive to the timelines. Regular meetings, either in person or by email/phone, and setting a goal of realistic expectations often help build a successful mentor-mentee relationship. In a fellowship training program, program directors and division chiefs can often facilitate an effective mentorship between the fellows and the faculty members.
Lack of funding has been identified as another significant barrier to research. Investigator-initiated clinical studies or basic science research mandates adequate funding. Observational studies like retrospective cohort studies, which are very popular among fellows, may not require funding per se. However, maintaining an infrastructure for such studies, which include preparing and maintaining databases, hiring research assistants and statisticians, etc., requires investment.1
Funding sources for research often include intramural grants. Graduate medical education dollars may also be used wisely to support trainee research.1 The National Cancer Institute (NCI) supports research and career development with a variety of awards (cancer.gov/grants-training). ASCO recognizes the need to support young investigators to produce the next generation of cancer researchers, and provides a number of grants and awards through the Conquer Cancer Foundation of ASCO.
Participation in research during fellowship can be a highly satisfactory experience for oncology fellows, and successful research experiences may produce accomplished physicianscientists. Both training programs and fellows need to identify the barriers to research and work together to create an environment that promotes intellectual curiosity, fosters original ideas, and implements effective methods to execute them.
References
- Rothberg MB. JAMA. 2012;308:2191-2.
- Rivera JA, Levine RB, Wright SM. J Gen Intern Med. 2005;20:366-9.
- Burns LJ, Clayton CP, George JN, et al. Acad Med. 2015;90:1061-6.
- Wong MD, Guerrero L, Sallam T, et al. J Grad Med Educ. 2016;8:85-90.
- Straus SE, Johnson MO, Marquez C, et al. Acad Med. 2013; 88:82-9.