Dec 20, 2017
In this issue’s Current Controversies in Oncology column, lymphoma expert Dr. Murali Janakiram, of Albert Einstein College of Medicine, answers a challenging clinical question posed by an attendee at a 2017 Best of ASCO® Meeting: Is there a role for maintenance lenalidomide after autologous hematopoietic stem cell transplantation in patients with relapsed diffuse large B-cell lymphoma?
By Murali Janakiram, MBBS, MD
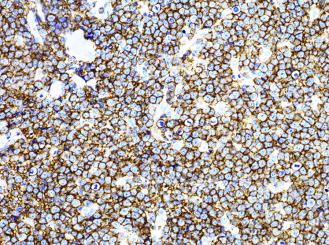
Lenalidomide has two main mechanisms of action in diffuse large B-cell lymphoma (DLBCL)—immunomodulatory and direct antineoplastic effects.1 Lenalidomide mediates increased natural killer cell activity, enhances antibody-dependent cellular cytotoxicity, and decreases pro-inflammatory cytokines in the tumor microenvironment. Lenalidomide also binds to the E3 ubiquitin ligase cereblon and decreases c-Myc and IRF4 expression, which in turn decreases nuclear factor–κβ and explains its preferential activity in activated B-cell DLBCL.
Lenalidomide has been effective as a single agent (overall response rate [ORR] 28%, complete response [CR] 7%)2 and in various combinations (cisplatin, cytarabine, and dexamethasone regimen; bendamustine; ibrutinib; rituximab) in relapsed/refractory DLBCL. As an upfront agent, lenalidomide with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP; together called R2-CHOP) produced high response rates (ORR 98%, CR 80%). The progression-free survival (PFS) and overall survival (OS) with R2-CHOP were similar between germinal center B-cell-like (GCB) and the more aggressive non-GCB subtype.3 A phase II/III trial that compared lenalidomide with and without R-CHOP in patients with unselected DLBCL (NCT01856192) or with activated B-cell DLBCL (NCT02285062) has been completed. Lenalidomide has reasonable activity in DLBCL and appears to mitigate the negative prognostic effect of non-GCB DLBCL.
There have been few maintenance studies in DLBCL, but no OS benefit has been observed in untreated or relapsed DLBCL with rituximab, enzastaurin, or everolimus. In this setting, data about lenalidomide maintenance are limited, especially in the autologous stem-cell transplantation (ASCT) setting.
The REMARC study is one of the largest studies to evaluate maintenance lenalidomide in patients between ages 60 and 80 years who had previously untreated DLBCL or other aggressive B-cell lymphoma.4 A total of 650 patients who had a CR or partial response after six or eight cycles of R-CHOP were randomly assigned to 25 mg/day of lenalidomide maintenance or to placebo for 21 days of every 28-day cycle for 24 months. With a median follow-up time of 39 months, the median PFS was not reached for lenalidomide maintenance, and it was 58.9 months for placebo (hazard ratio [HR] 0.708; p = 0.01). At 52 months, OS was similar between arms (HR 1.218; p = 0.26). The most common grade 3 and grade 4 adverse events associated with lenalidomide versus placebo were neutropenia (56% vs. 22%) and cutaneous reactions (5% vs. 1%), respectively. Interestingly, the median PFS was in favor of lenalidomide in the GCB arm but not in the non-GCB arm when compared with placebo. The rate of second primary malignancies was similar in both arms.
In another small, multicenter, phase II study, 25 mg/day of lenalidomide maintenance was given to 48 patients with chemosensitive relapsed DLBCL who were not eligible for ASCT or who had experienced relapse after ASCT.5 After a mean of 12 cycles in a median of 25 months of treatment, the 1-year PFS was 70%. Grade 3 to 4 neutropenia was the most common toxicity in this trial. Overall, these results suggest that maintenance lenalidomide can improve PFS in select high-risk patients with treated DLBCL.
Very few trials of lenalidomide maintenance in the post-ASCT setting have been reported. Feldman et al6 conducted a phase I/II trial of lenalidomide plus rituximab, ifosfamide, carboplatin, and etoposide (RICE) followed by ASCT and lenalidomide maintenance after ASCT. In this trial, no dose reductions in lenalidomide or RICE were needed, and 10 patients underwent ASCT. In eight of the 10 patients who started maintenance lenalidomide, only three patients remained on maintenance lenalidomide (one patient completed treatment, and two had ongoing treatment). The most common reason for noncompletion of maintenance was disease progression. As expected, neutropenia was the most common toxicity observed with lenalidomide. Interestingly, the response rate of GCB DLBCL was higher than that of non-GCB DLBCL in this study. Because of the small numbers in this study, no definitive conclusions about maintenance lenalidomide could be drawn.
Svoboda et al7 reported interim results of a phase I/II prospective, open-label trial of lenalidomide maintenance after ASCT in patients with lymphoma who were at high risk for relapse, as defined by residual FDG-PET–positive lesions (standardized uptake value > 2.5) immediately before ASCT. Lenalidomide was initiated 28 to 100 days after ASCT and was planned for up to 24 cycles. Of the 11 evaluable patients, eight (73%) had DLBCL (four had GCB and four had non-GCB disease). The median time on lenalidomide was 13 cycles (range, one to 24 cycles), and the dose of 10 mg/day was determined to be appropriate for phase II. Most patients (55%) discontinued lenalidomide because of disease progression, and one discontinued because of a grade 3 rash possibly related to lenalidomide. One patient developed adenocarcinoma of the colon 1 year after completion of lenalidomide, and one patient developed therapy-related acute myeloid leukemia 10 months after lenalidomide discontinuation. At a median follow-up time of 2 years, the PFS of the complete cohort was 62.3%, and the OS was 75.0%. This trial suggests that maintenance lenalidomide is feasible after ASCT for lymphoma and that the median PFS is improved with lenalidomide maintenance. The most common adverse effects were neutropenia and rash in this setting, and the most common reason for discontinuation was disease progression.
Overall, these trials suggest that lenalidomide maintenance is feasible and can increase PFS in select high-risk patients after ASCT. Neutropenia and skin rash are the most likely adverse effects encountered. Whether secondary malignancies, especially therapy-related acute myeloid leukemia, could be increased in this setting, because most people would have received several cycles of high-dose chemotherapy, remains to be seen. It is likely that, in the maintenance setting, the immunomodulatory effect would be more important, because most of these studies in the maintenance setting favor the GCB subtype. At this time, in the absence of phase II data or randomized trials, it is difficult to recommend maintenance lenalidomide after ASCT while additional trials in this area are needed.
References
- Gribben JG, Fowler N, Morschhauser F. J Clin Oncol. 2015;33:2803-11.
- Witzig TE, Vose JM, Zinzani PL, et al. Ann Oncol. 2011;22:1622-7.
- Nowakowski GS, LaPlant B, Macon WR, et al. J Clin Oncol. 2015;33:251-7.
- Thieblemont C, Tilly H, Gomes da Silva M, et al. J Clin Oncol. 2017;35:2473-81.
- Ferreri AJ, Sassone M, Zaja F, et al. Lancet Haematol. 2017;4:e137-46.
- Feldman T, Mato AR, Chow KF, et al. Br J Haematol. 2014;166:77-83.
- Svoboda J, Strelec LE, Landsburg DJ, et al. Blood. 2016;128:4639.