By Samer Al Hadidi, MD, MS, FACP
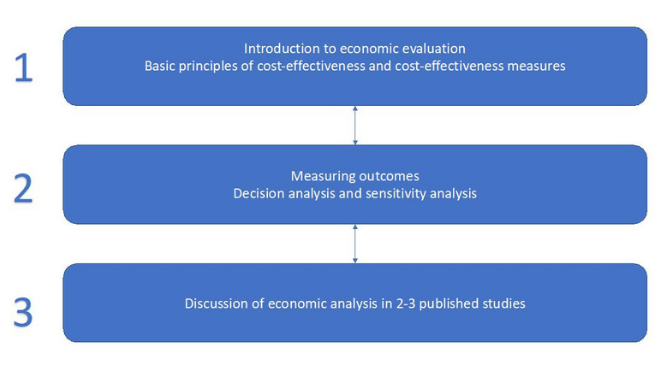
The list of options of cancer therapeutics continue to grow. While adding more effective choices to treat patients with cancer is exciting, the cost of cancer care is becoming more problematic.1 The Accreditation Council for Graduate Medical Education (ACGME) requires faculty members involved in graduate medical training in hematology, as well as medical oncology, to be able to demonstrate commitment to the delivery of safe, high-quality, cost-effective, patient-centered care as one of the training core measures.2 However, formal training in cost-effectiveness is not usually required for either faculty members or trainees. Implementation of a well-structured, oncology-based cost-effectiveness training for both faculty members and trainees will be of paramount importance and should be prioritized as a significant urgent change in training curriculum.
Economic efficiency is important when evaluating medical treatments. Cost is not only about the price of a drug or intervention. It includes many other aspects that are either related to patients or healthcare systems. Economic efficiency simply asks the question: Are we getting the best outcome for the expenditure? Or are we minimizing cost for the outcome achieved? While the vast majority will agree that human life is priceless, most of the approved cancer drugs in the recent years are based on cancer control rather than overall survival.3 Better cancer control may lead to improved survival or quality of life; however, this is not necessarily true and is extremely variable between different cancers, patients and treatment options.
References
- Kantarjian H, Rajkumar SV. Why are cancer drugs so expensive in the United States, and what are the solutions? Mayo Clin Proc. 2015 Apr;90(4):500-4. DOI: https://doi.org/10.1016/j.mayocp.2015.01.014
- ACGME Program Requirements for Graduate Medical Education in Hematology and Medical Oncology. Available at: www.acgme.org/Portals/0/PFAssets/ProgramRequirements/155_HematologyAndMedicalOncology_2020.pdf?ver=2020-06-29-162353-163. Accessed 27 April 2021.
- Kim C, Prasad V. Cancer Drugs Approved on the Basis of a Surrogate End Point and Subsequent Overall Survival: An Analysis of 5 Years of US Food and Drug Administration Approvals. JAMA Intern Med. 2015 Dec;175(12):1992-4. DOI: https://doi.org/10.1001/jamainternmed.2015.5868
- Schnipper LE, Davidson NE, Wollins DS, et al. American Society of Clinical Oncology. American Society of Clinical Oncology Statement: A Conceptual Framework to Assess the Value of Cancer Treatment Options. J Clin Oncol. 2015 Aug 10;33(23):2563-77. DOI: https://doi.org/10.1200/jco.2015.61.6706
- Schnipper LE, Davidson NE, Wollins DS, et al. Updating the American Society of Clinical Oncology Value Framework: Revisions and Reflections in Response to Comments Received. J Clin Oncol. 2016 Aug 20;34(24):2925-34. DOI: https://doi.org/10.1200/jco.2016.68.2518
- What is the CEAR Registry. Available at https://research.tufts-nemc.org/cear4/AboutUs/WhatistheCEARegistry.aspx. Accessed 27 April 2021.


Comments
Peter Paul Yu, MD, FASCO, FACP
May, 08 2021 11:10 AM
Thank you Samer for articulating the need to raise awareness among oncology fellows on science based methods to assses "value". ICERs have been mostly used in countries where the national healthcare budget is fixed. In the U.S. where healthcare is a considered an entitlement without a fixed national Medicare budget, we have largely avoided discussions about comparative effectieness and impact on the national budget. However, ICERs have limitations, In particular, the calcuation of "disutilities", which are how the negative impact on QOL is measured, are not onoclogy derived and need to be better defined for the cancer population https://jitc.bmj.com/content/jitc/7/1/235.full.pdf
Samer Al Hadidi, FACP, MD, MS
May, 22 2021 10:46 PM
Thank you Dr Yu for sharing the article and thoughtful comment. I totally agree with you, I hope the oncology community will work to better define cost-effectivness measures.
Samer