By Shaalan Beg, MD, MBA, FASCO, and Noelle K. LoConte, MD, FASCO
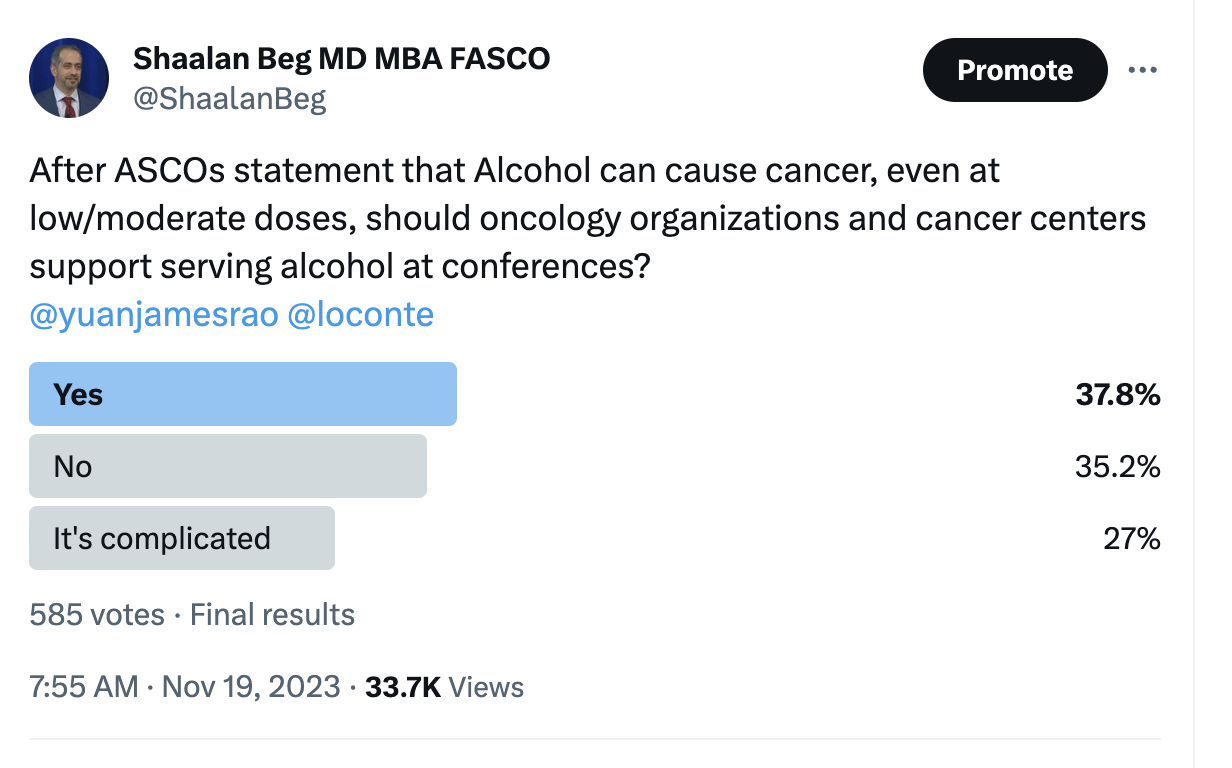
Should oncology organizations and cancer centers allocate funds to serve and therefore promote the consumption of alcohol, a known carcinogen? According to a recent poll on social media, only approximately one-third of respondents believe they should.1
This topic has sparked numerous discussions, and these discussions can be broadly categorized into three main issues:
- The lack of robust data establishing a clear causation between alcohol and cancer
- The argument that the decision to consume alcohol is a personal one
- The presence of various other risk factors for cancer, prompting the question of where an organization's responsibility begins and ends
ASCO released a policy statement on alcohol in 2017; that paper is one of the most highly viewed and downloaded manuscripts for the Journal of Clinical Oncology, with over 3.2 million downloads.2 This paper has also remained as one of the “Most Viewed in the Last 60 Days” papers on the JCO website since publication over 6 years ago. It is estimated that 4% to 5% of cancers globally are associated with alcohol use. According to the World Health Organization there are seven cancers which are currently determined to be at least partially caused by alcohol consumption.3 It is estimated that while there is a clear dose-related relationship between alcohol consumption and higher rates of these cancers, in some cancers even low to moderate consumption (as little as one drink per day) has been associated with an increased risk of malignancy.
The discussion on serving alcohol at oncology events focuses on whether these organizations, with a mission to reduce the burden of cancer across the world, should allocate funds to disseminate a potential carcinogen. It does not impact personal freedom to drink alcohol, nor does it suggest limits on individuals purchasing alcohol at events. The analogy of smoking tobacco products is often brought up in this discussion. Smoking differs from alcohol consumption because smoking poses the added risk of passive smoke to nonsmokers. It is this point which made it easier to advocate for change in laws that banned smoking in many public places. This caused the perception of smoking to change in the public’s eye and allowed subsequent limits being imposed on advertisements on television and at sporting events. This impacted the social acceptance of smoking in the U.S., which contributed to impressive reductions in smoking-related diseases over the years. So, it's fair to ask: what is the message being relayed to the community about the role of alcohol and cancer if oncology organizations purchase and distribute alcoholic drinks at their events?
The decision on whether to consume alcohol, or how much to consume, is not simply a matter of personal choice. Unlike most other cancer risk factors, alcohol consumption has additional challenges which impact someone's risk of exposure. It is estimated that 10% to 13% of the general population may struggle with alcohol dependency at some point in their life.4 At a conference of 35,000 attendees, that is more than 3,500 people who may have personal struggles with alcohol consumption at some point in their life, with additional people knowing others who have. Easy access to alcohol can lead to increased consumption.
In a world with many potential cancer risk factors, how does a health care organization decide if a particular risk factor meets the bar? The question is not whether oncology organizations should “ban” other risk factors such as sugary drinks at their events. (What about sunlight?) Instead, one might similarly ask whether oncology organizations and cancer centers should provide cigarettes and tanning beds for their conference attendees. When it comes to deciding which risk factors are worthy of imposing limitations, such decisions are not much different than others we face in medicine every day. We should rely on the evidence. When it comes to alcohol use and cancer, one can review the evidence that led to ASCO releasing its position statement in 2017.
One potential approach is to reconsider the practice of serving complimentary alcoholic beverages at conferences, and instead offer attendees the option to make individual purchases. Additionally, societies could implement drink limits through tickets or coupons. Oncology meetings could diversify their refreshment menus by incorporating a broader selection of non-alcoholic options, such as mocktails. Such a shift promotes a more inclusive environment and helps send a clear message that oncology groups do not endorse a potential carcinogen.
Health care conferences are an important venue to network with others and share ideas. In many countries, alcohol has a cultural and social role in building relationship. For many individuals, an occasional alcoholic beverage is a safe way to relax after work and connect with others. Attendance and engagement in meetings can also increase when alcohol is being served, which can increase the value of the event. The discussion surrounding whether oncology organizations should purchase and serve alcohol at events underscores the balance between the cultural and social roles of alcohol, evidenced-based decision-making, and the responsibility of organizations. It's also important to consider the potential carcinogenic effects of alcohol and draw lessons from analogous situations in the past.
Is this just petty virtue signaling, or when it comes to alcohol and cancer, do signals matter?
Dr. Beg is an adjunct associate professor at UT Southwestern Medical Center. Disclosure.
Dr. LoConte is a medical oncologist and geriatrician with a clinical interest in gastrointestinal malignancies. Disclosure.
References
- Shaalan Beg (@ShaalanBeg). “After ASCOs statement that Alcohol can cause cancer, even at low/moderate doses, should oncology organizations and cancer centers support serving alcohol at conferences? @yuanjamesrao @loconte.” Twitter. Nov 19, 2023. Accessed Nov 20, 2023.
- LoConte NK, Brewster AM, Kaur JS, et al. Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. J Clin Oncol. 2018 Jan 1;36:83-93. doi: 10.1200/JCO.2017.76.1155.
- Kluge HHP, Weiderpass E. Joint statement by WHO/Europe and IARC to the European Parliament – raising awareness of the link between alcohol and cancer. World Health Organization. Nov 6, 2023. Accessed Jan 25, 2024.
- Section 2 PE Tables. Results from the 2022 National Survey on Drug Use and Health: Detailed Tables, SAMHSA, CBHSQ. Accessed Jan 25, 2024.



Recent posts