Jul 09, 2021
By Jo Cavallo, The ASCO Post
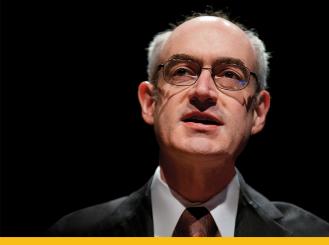
Internationally renowned for his pioneering research in combining high-dose radiation therapy and chemotherapy in the treatment of locally advanced head and neck cancer to improve patient survival, Everett E. Vokes, MD, FASCO, is dedicating his tenure as 2021-2022 ASCO president to expanding ASCO’s global reach and advancing lessons learned from the COVID-19 pandemic to improve cancer care for all patients.
Born in New York City in 1954, Dr. Vokes, the John E. Ultmann Professor, chair of the Department of Medicine, and physician-in-chief of the University of Chicago Medicine and Biological Sciences, later moved with his mother to Bonn, West Germany, and received his medical degree at the University of Bonn Medical School. He returned to the United States to complete his residency in internal medicine at Ravenswood Hospital Medical Center in Chicago and at the University of Southern California in Los Angeles.
During his fellowship training at the University of Chicago, Dr. Vokes hypothesized that combining radiation therapy and chemotherapy might lead to a cure in some advanced cancers. This theory would be validated in his subsequent research testing various induction chemotherapies and regimens of concurrent radiotherapy; they have since been shown to increase cure rates in advanced head and neck cancers, non-small cell lung cancer, esophageal cancer, and other solid tumors. In addition to his clinical and translational research in head and neck cancers, Dr. Vokes is investigating new active therapeutic agents, as well as the interaction of chemotherapy and radiation therapy, in lung cancers.
After completing his residency at the University of Southern California, in 1983, Dr. Vokes furthered his training as a hematology/oncology fellow at the University of Chicago. He later joined the faculty and was promoted to professor in 1995. He then served as chief of the Section of Hematology/Oncology and is currently chair of the Department of Medicine at the institution. From 1994 to 2009, Dr. Vokes was the principal investigator of the University of Chicago’s National Cancer Institute–funded phase II network and served as chair of the Cancer and Leukemia Group B Respiratory Committee (now part of the Alliance for Clinical Trials in Oncology) from 2004 to 2017.
In recognition of his research accomplishments in a career spanning 35 years, Dr. Vokes has received ASCO’s Translational Research Professorship; a grant for research on malignancies of the upper aerodigestive tract from the Francis L. Lederer Foundation; and, in 2013, OncLive’s Giants of Cancer Care Award.
An ASCO member since 1986, Dr. Vokes has served the Society in many roles, including chair of the Annual Meeting Education Committee and member of the Annual Meeting Scientific Program Committee, the Conquer Cancer Development and Fundraising Committee, the Cancer.Net Editorial Board, and the ASCO Nominating Committee. He was a member of ASCO’s Board of Directors from 2009 to 2012. He began his term as ASCO president on June 8, 2021, after serving for a year as president-elect.
What goals do you hope to accomplish during your tenure as ASCO president?
EV: ASCO plans to become more engaged globally, and my presidential theme, “Advancing Equitable Cancer Care Through Innovation,” captures the potential long-term impact of innovations in cancer care we have seen over the past year due to the COVID-19 pandemic that could benefit patients worldwide. I would like to work on some of those innovations that forced change on society at large—and, of course, on our profession—that might otherwise have taken much longer if it had not been for the pandemic.
At the top of the list is telemedicine, which has the potential to improve cancer care in terms of health equity and access, and, hopefully, in clinical trial participation as well. Telemedicine also allows global outreach to share medical opinions, broaden educational forums, and expand access to research data. There are still issues to be resolved, including reforms to enable physicians in the United States, and potentially in other countries, to practice medicine across states and national borders. In addition, significant financial investment will be needed to develop telemedicine capabilities worldwide and to accommodate the different needs of developed and developing medical systems. The potential of telemedicine is very clear. It would allow us to reach people anywhere in the world, including in both urban and rural areas.
Clearly, poverty and lack of access to broadband technology are barriers to accessing telemedicine for some patients, and these challenges will need to be addressed. At the University of Chicago Medicine, for example, we have significant outreach programs to patients living on the South Side of the city. In my experience, although sometimes a video visit has to be changed to a telephone call, in the end, we are making contact with patients we might not have made otherwise.
Telemedicine is also spurring innovation in remote clinical trial enrollment, and I think this is an area that could be expanded. In addition, we have to review the merits of clinical trial eligibility criteria for new drugs. However, this technology allows us to broaden enrollment to include patients with varying demographics and widespread geographic locations. Providing telemedicine capabilities has taught us how to bring care to the patient rather than always needing the patient to visit the site of care.
The use of artificial intelligence in cancer diagnostics has also gained momentum over the past year. I think in time, this technology will allow sophisticated algorithms to quickly interpret tissue specimens and replace genomic evaluations.
Your medical specialty is in the clinical care and translational research of head and neck and lung cancers, which have seen dramatic improvements in patient outcomes. How might your expertise in these cancers influence your agenda as ASCO president?
EV: Everything I have done in research and in the clinical care of patients with these cancers has involved teamwork. What we do to optimize outcomes always involves consultations with our colleagues in radiation oncology, surgery, pathology, and other specialties. For patients with head and neck cancers, we include discussions with dentists, speech, and swallowing experts, among others. Of course, in lung cancer, we also consult with pulmonary specialists. We also collaborate with pathologists and apply modern genetics to make the most accurate diagnosis possible.
What we do at ASCO also involves teamwork. We are a broad organization that uniquely includes all specialties involved in cancer care and broad participation from all of those specialties, as reflected in the program developed for the Annual Meeting.
I have been involved with ASCO throughout my entire professional career, and it has given me exposure to highly impactful and dedicated role models in a field that 30 or 40 years ago was still looked upon with skepticism. To see the progress in scientific innovation that has advanced diagnostics and therapeutics over this time is amazing.
The focus of 2020-2021 ASCO president Dr. Lori J. Pierce’s presidential term has been on health equity for all patients, everywhere. Reducing or eliminating cancer disparities in minority communities is daunting and requires changes in public policy, accessibility to health insurance and high-quality cancer care, and increased awareness of prevention strategies. How might you continue and strengthen ASCO’s efforts to ensure health equity for all patients?
EV: Dr. Pierce’s work on health equity is deeply ingrained into the structure of the organization and will leave a lasting mark on ASCO. There is a very natural continuation of Dr. Pierce’s presidential theme in my theme. My goal is to make it possible to expand access to cancer care through telemedicine, improve care delivery models, and increase participation in clinical trials, especially for underserved populations, globally and locally in the United States. Looking at global cancer care through innovation is perfectly suited to continuing Dr. Pierce’s theme of equity for all patients, everywhere.
What are some of the greatest challenges facing the oncology community over the next 5 years to advance cancer progress? How will ASCO continue to help oncologists meet these challenges?
EV: The challenges we face in the near future will center on improving cancer prevention strategies, including healthier diets, increased physical activity, appropriate and timely screenings, and immunization against human papillomavirus and hepatitis. The other big issue facing oncology is the increasing financial toxicity linked to modern care and therapeutics. As more effective drugs become available, the access to those drugs and the associated costs of administering them will continue to be a challenge.
Another significant challenge will be to increase and train the next generation of oncologists and scientists. Currently, there is high enthusiasm for the field of oncology among residents, and we need to nurture that enthusiasm with mentoring and support for our fellows and young faculty.
For me personally, as well as for ASCO, mentoring the next generation of clinician/researchers has always been a priority, and that commitment will continue. This is reflected by ASCO’s expansive portfolio of Young Investigator and Career Development Awards.
Approximately one-third of ASCO members practice outside of the United States, and one-quarter practice in low- and middle-income countries. Do you have plans to expand ASCO’s global cancer programs, especially in resource-limited countries?
EV: ASCO intends to connect with oncologists throughout the world. In 2019, ASCO launched the Asia Pacific Regional Council, which is made up of a group of distinguished oncology leaders from countries in the Asia Pacific region, to facilitate and encourage member involvement in ASCO’s global activities. The council was instrumental in assisting with the launch that year of ASCO Breakthrough, a global meeting of advanced technology and cancer care, which was held in Bangkok. The meeting attracted nearly 500 attendees representing more than 30 countries from a variety of disciplines, including information and computer science, artificial intelligence, basic and translational research, social media, and biomedical engineering.
The second ASCO Breakthrough meeting, originally scheduled for later this year, has been postponed due to the ongoing COVID-19 pandemic. It will be held on August 25-27, 2022, in Yokohama, Japan. ASCO has also organized a Latin America Regional Council this year to deepen its engagement with ASCO members in that region as well as to address the specific needs and challenges of oncology professionals from that region of the world.
In the coming years, ASCO will be moving more and more in the direction of engaging oncology leaders throughout the world to help guide ASCO and its international events. Through Conquer Cancer, the ASCO Foundation, ASCO has established the Long-Term International Fellowship, which provides early-career oncologists in low- and middle-income countries the support and resources needed to advance their training through mentors in the United States, Canada, and Europe. ASCO also provides research funding through its International Innovation Grant to support innovative projects that may have a significant impact on cancer control in low-resource countries.
Although the COVID-19 pandemic has presented us with many challenges this year, it has also presented the opportunity to broaden our outreach to the global oncology community through the ASCO Annual Meeting, which was held virtually in 2020 and 2021. Of course, we all want to get together in person to be able to have a direct exchange of ideas and to get to know one another better; however, due to the pandemic, ASCO opted to make the meeting available to all members virtually, which further increased participation this past year.
Hybrid meetings that combine an in-person component with a virtual experience may eventually be the optimal approach. Although there is much benefit from in-person meetings, providing virtual access to new information globally is invaluable.
What enduring legacy would you like to leave with the Society?
EV: It has been a rewarding professional experience to be part of this amazing, multispecialty organization. It has always fostered innovation and discovery; served to present and publish new knowledge; promoted the application of new knowledge in patient care; and embraced the importance of mentoring and supporting the next generation of oncology clinical care providers and researchers.
However, in the end, our main focus is really all about individual patients and their treatment, their dignity, and their future. I hope that during my presidential year, we will continue to further advance patient care, so more patients are cured, and every survivor can live a high-quality life after cancer.
Originally published in The ASCO Post; adapted and reprinted with permission.