 By Barbara K. Rimer, DrPH
By Barbara K. Rimer, DrPH
Chair, President’s Cancer Panel
Dean and Alumni Distinguished Professor, UNC Gillings School of Global Public Health
In September 2017, ASCO issued guidelines to improve patient-clinician communication.1 The framework offers cancer clinicians concrete practices to help them deliver complex treatment information more effectively to patients and their families and caregivers to support informed decision making.
This guidance comes at a good time. Evidence is growing that effective communication plays a key role in high-quality care delivery and outcomes, particularly in oncology, where patients and their caregivers must navigate a complex web of treatment options, instructions, appointments, and providers. Many clinicians, however, have had minimal training on how to communicate health information in a manner that patients understand and retain and that is culturally appropriate.
The guidelines identify appropriate practices based on evidence to use in approaching challenging discussions about recommended treatment options, goals of treatment, prognosis, facilitating family involvement in care, and end-of-life preferences. They also make a strong recommendation that clinicians address patients’ concerns about treatment costs.
Actions recently highlighted by the President’s Cancer Panel are aligned with ASCO’s recommendation that patients be informed about the costs of care as part of the treatment decision-making process. Costs—particularly out-of-pocket costs for drugs—should be an essential component of patient-clinician communication.
Our latest report to the president, Promoting Value, Affordability, and Innovation in Cancer Drug Treatment,2 released on March 13, outlines six critical action items aimed at growing a robust pipeline of innovative cancer drugs and ensuring that they are accessible to and affordable for those who need them. One recommendation urgently calls on ASCO members and their colleagues to take action:
Enable meaningful communication about treatment options,
including cost information,
to support patients’ decision making.
We were fortunate that ASCO CEO Clifford A. Hudis, MD, FACP, FASCO, provided the critical perspective of clinical oncologists during the report development process. He was part of a group of stakeholders that included patients, clinicians, government officials, and leaders from the pharmaceutical and insurance industries that we gathered for workshops where we discussed and debated important questions about cancer drug costs and cancer care overall.
Cancer Drug Innovation Comes at a High Price to Patients
It is an exciting time for cancer drug innovation. Some new cancer drugs have been transformative, offering patients a chance at long-term remissions, even cures. A robust cancer drug pipeline is essential to continuing—even accelerating—the progress that our biomedical research enterprise has recently made against the disease. During our workshops, we heard from patients who expressed gratitude that innovative drugs offered them options they would not have had even a few years ago. However, it cannot be ignored that spending on cancer drugs is straining patients’ and society’s resources and is a major cause for concern, particularly since the number of cancer cases is expected to rise as the U.S. population ages.3 Virtually all new cancer drugs enter the market with price tags of $100,000 or more per year,4 and launch prices of $400,000 for a year of treatment are becoming a new reality. Prices are similarly high for novel drugs and the “me-too” drugs that often follow,4,5 and prices often increase substantially after launch.6
It’s not surprising that more than 90% of Americans in ASCO’s nationally representative survey said that cancer drugs are too expensive.7
Drug costs are accelerating far faster than costs for other components of care,8 which together, can place a heavy financial burden on patients and their families. When financial resources are strained, patients are less likely to follow medication regimens, threatening the effectiveness of treatment. The negative and often profound impact that cancer treatment costs can have on patients and their families and caregivers is referred to as financial toxicity.9 Patients who experience financial toxicity appear to experience worse outcomes than those who do not, although the specific cause is not known
An urgent need is emerging to ensure that drug prices are aligned with the value provided to patients. High prices may be warranted for innovative drugs that significantly extend survival and/or substantially improve quality of life, but many do not provide clinically meaningful improvements as defined by ASCO.10 In our report, we concluded that a first step toward paying for value is to develop a framework for value-based pricing, including a shared definition of value. The goal is to ensure that highly effective cancer drugs are accessible to patients regardless of cost, while drugs that provide little or no benefit might not be reimbursed in the same way.
“Precision” Communication With Patients Should Include Cost
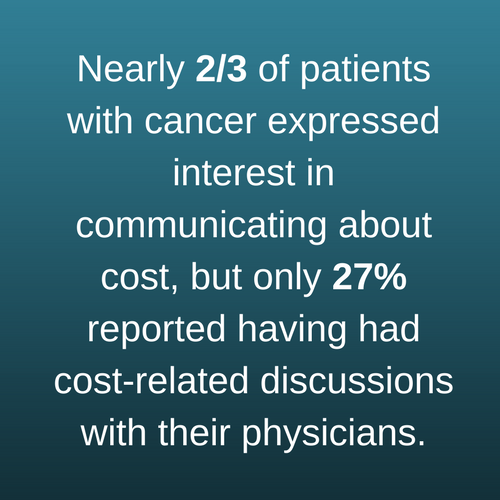 Historically, discussions about cost have not been part of routine clinical care for cancer. During the workshops we held with stakeholders to gather input for this report, we heard that oncologists are often uncomfortable introducing cost into discussions with patients and families. One survey found that nearly two-thirds of patients with cancer expressed interest in communicating about cost, and most oncologists agreed that patients should understand the financial implications of their treatment options.11 Despite this, discussions about cost are infrequent—only 27% of patients with cancer and less than half of oncologists surveyed reported having had cost-related discussions.
Historically, discussions about cost have not been part of routine clinical care for cancer. During the workshops we held with stakeholders to gather input for this report, we heard that oncologists are often uncomfortable introducing cost into discussions with patients and families. One survey found that nearly two-thirds of patients with cancer expressed interest in communicating about cost, and most oncologists agreed that patients should understand the financial implications of their treatment options.11 Despite this, discussions about cost are infrequent—only 27% of patients with cancer and less than half of oncologists surveyed reported having had cost-related discussions.
This hesitancy is understandable. Lack of transparency often makes it difficult to know how much patients will be charged for drugs and other components of care and the portion they will be responsible to pay out of pocket.12,13 Physicians want their patients to receive the best possible therapy regardless of cost. However, it’s clear that patients want and need cost information to help them plan accordingly. Yousef Zafar, MD, MHS, of Duke Cancer Center, said during one workshop, “Cost is another side effect of treatment…in terms of communicating treatment benefit, we’ve got to realize that the oncologist has to have some role, even if it’s just screening [for financial toxicity].”
The Panel concluded that patients and their families should be offered conversations about the potential costs of drugs and other care. After discussion with their cancer care teams, patients should be empowered to identify and select treatments aligned with their needs, values, and preferences. To accomplish this, patients and their families need:
- Accurate information about their diagnosis and prognosis;
- Clear understanding of recommended treatment options, including treatment purpose (e.g., cure, extended survival, palliation);
- Realistic expectations about possible clinical benefits and harms of treatment options; and
- Access to information about costs of drugs and other treatment options, including both direct and indirect costs.
Cancer clinicians should tailor this information to the needs, preferences, and comprehension capacity of individual patients. Such precision communication is essential to patient-centered cancer care.
Closing Knowledge Gaps and Providing Tools to Facilitate Cost Discussions
The Panel concluded that access to cost information could enable patients to integrate financial considerations, as they desire, into their personal value assessments of treatment options. Cost information also may help patients, families, and care teams identify ways to prevent or address financial toxicity. However, many unanswered questions remain regarding the effects these discussions may have on clinical decision-making and outcomes, as well as patients’ quality of life, well-being, satisfaction, and financial toxicity. Similarly, it is not yet known which member of the care team is best suited to have cost discussions with patients and their families.
We commend the work of several groups—including ASCO and the National Comprehensive Cancer Network—that have begun developing tools to help clinicians and patients incorporate cost into cancer treatment decisions.14,15 Tools and strategies should be evaluated to determine whether they result in improved communication and decision-making. And they should be optimized for easy integration into clinical workflows and tailored to the specific circumstances of individual patients. Patients and other stakeholders are counting on ASCO members and other cancer clinicians to use these emerging resources to gain the knowledge and communication skills needed to approach cost discussions.
Urgent Collaborative Action Needed on Escalating Drug Prices
Throughout the development of our report, we observed widespread agreement among stakeholders that rising cancer drug prices are a burden on patients and are straining health system and societal resources. Ensuring clear communication between clinicians and patients on potential financial effects of treatment is one of several urgent actions we recommend that will move us closer to the goal of affordable access to high-value cancer drugs for all patients who need them.
A noted leader in cancer prevention and control and health communications, Dr. Rimer was appointed to the President's Cancer Panel by President Barack Obama in 2011. Dr. Rimer's work in the cancer field has guided national research, practice, and policy for more than 20 years. Her research has contributed to the evidence base in a number of cancer-related areas, including informed decision making, long-term maintenance of behavior changes, adherence to cancer prevention and early detection practices, and dissemination and implementation of evidence-based interventions. Dr. Rimer received a BA and an MPH from the University of Michigan and a DrPH from the Johns Hopkins School of Hygiene and Public Health.
References
- Gilligan T, et al. Patient-clinician communication: American Society of Clinical Oncology Consensus Guideline. J Clin Oncol. 2017;35:3618-32. Available from: https://www.asco.org/practice-guidelines/quality-guidelines/guidelines/supportive-care-and-treatment-related-issues#/27581.
- Promoting Value, Affordability, and Innovation in Cancer Drug Treatment. A Report to the President of the United States from the President’s Cancer Panel. Bethesda (MD): President’s Cancer Panel; 2018 March. Available from: https://prescancerpanel.cancer.gov/report/drugvalue/.
- Weir HK, Thompson TD, Soman A, Moller B, Leadbetter S. The past, present, and future of cancer incidence in the United States: 1975 through 2020. Cancer. 2015;121:1827-37. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25649671.
- Mailankody S, Prasad V. Five years of cancer drug approvals: innovation, efficacy, and costs. JAMA Oncol. 2015;1:539-40. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26181265.
- Fojo T, Mailankody S, Lo A. Unintended consequences of expensive cancer therapeutics-the pursuit of marginal indications and a me-too mentality that stifles innovation and creativity: the John Conley Lecture. JAMA Otolaryngol Head Neck Surg. 2014;140:1225-36. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25068501.
- Bennette CS, Richards C, Sullivan SD, Ramsey SD. Steady increase in prices for oral anticancer drugs after market launch suggests a lack of competitive pressure. Health Aff (Millwood). 2016;35:805-12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27140986.
- American Society of Clinical Oncology. National Cancer Opinion Survey: key findings. Alexandria (VA): ASCO; 2017 Oct 24. Available from: https://www.asco.org/sites/new-www.asco.org/files/content-files/research-and-progress/documents/ASCO-National-Cancer-Opinion-Index-infographic.pdf.
- Fitch K, Pelizzari PM, Pyenson B. Cost drivers of cancer care: a retrospective analysis of Medicare and commercially insured population claim data 2004-2014. Milliman (commissioned by the Community Oncology Alliance); 2016 Apr. Available from: http://www.milliman.com/insight/2016/Cost-drivers-of-cancer-care-A-retrospective-analysis-of-Medicare-and-commercially-insured-population-claim-data-2004-2014.
- PDQ Adult Treatment Editorial Board. Financial toxicity and cancer treatment. Bethesda (MD): National Cancer Institute. Available from: https://www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-hp-pdq.
- Kumar H, Fojo T, Mailankody S. An appraisal of clinically meaningful outcomes guidelines for oncology clinical trials. JAMA Oncol. 2016;2:1238-40. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27281466.
- Shih YT, Chien CR. A review of cost communication in oncology: patient attitude, provider acceptance, and outcome assessment. Cancer. 2017;123:928-39. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27893929.
- Association of Community Cancer Centers. 2016 trends in cancer programs. Rockville (MD): ACCC; 2016. Available from: http://www.accc-cancer.org/surveys/pdf/Trends-in-Cancer-Programs-2016.pdf.
- Robert Wood Johnson Foundation. How price transparency can control the cost of health care. Health Policy Snapshot Series. Princeton (NJ): RWJF; 2016. Available from: https://www.rwjf.org/en/library/research/2016/03/how-price-transparency-controls-health-care-cost.html.
- American Society of Clinical Oncology. ASCO Value Framework. Alexandria (VA): ASCO; 2016. Available from: https://www.asco.org/practice-guidelines/cancer-care-initiatives/value-cancer-care
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) with NCCN Evidence Blocks™. Fort Washington (PA). Available from: https://www.nccn.org/evidenceblocks/default.aspx.


Comments
Joel M. Schindler, PhD
Apr, 16 2018 3:11 PM
Our organization has actually conducted research with cancer patients on their perceptions of drug costs, the risk of not being compliant and the impact of oncology drug costs on their compliance. The results are srartling with a majority claiming costs require fiancial adjustments and a third claiming signfincat financial changes needed to be made. The toxicity is far geater than one might think. The results are presented here:
https://www.mv-research.com/images/pdfs/cancer_drug_costs_and_risk.pdf