The most exciting and difficult part of my job is keeping up with all the rapid changes occurring in the field of cancer treatments. It is amazing how each day there seems to be a breakthrough treatment coming along, shifting old cancer paradigms. Although this is a good problem to have, finding time to stay current is easier said than done.
Even more difficult is making sure we can explain these new changes to our patients so they are educated and informed. I believe effective patient education is essential for any doctor, irrespective of the field of medicine or practice setting. Trying to explain immunotherapy to one of my patients demonstrated to me the importance of developing this skill for all my future patients.
I met this particular patient after a long day of hospital rounds. I was on consults and, as usual, the annoying ring of the pager went off right as I was ready to leave for the day. I spoke to the hospitalist about a young man with metastatic bladder cancer. Unfortunately, the patient had a new spot in his bone that was causing unrelenting pain. Six months prior he had undergone chemotherapy and then removal of his bladder and was full of hope for staying in remission. This hope was shattered when he discovered the cancer had returned with a vengeance, attacking his bones and strength.
When I entered the room, I quickly realized this would take some time. He was on his laptop and random medical journals lined his bed. Multiple family members were present, simultaneously looking at me and at their mobile devices, presumably searching for answers. I started to speak and, after pleasant introductions, he asked, “Doctor, is it ok if I record our conversation? I am an accountant so I like to document everything.”
I responded, “Of course. Actually, I encourage it. I can use it as evidence that I’m not avoiding my in-laws, who are visiting this weekend.”
Luckily, this broke the ice and the people in the room smiled. They put down their phones and were now eager to be engaged in the conversation. We talked and discussed what would be the best plan. Radiation would be used to treat his pain, but we also needed to come up with a plan to attack the cancer spreading through his body. I explained that there is new promising data utilizing our own T cells to fight cancer, called checkpoint inhibitors.
He responded, “Doctor, I have tried to learn about these drugs since they are everywhere in the press, yet I have no idea how it works. Can you break it down for me, like you would for your kids?”
This is a common dilemma we all face in medicine. How do we best explain what we are doing to our patients? From the ER doctor about to do a procedure to the surgeon about to operate, we are all faced with educating our patients in simple, understandable terms. If we fail to do this, then we in essence have not fulfilled our responsibility to our patients.
When we are at the bedside, eye to eye with the patient and their families, we can do more than any website, journal, or even Dr. Google can to help our patients. Making simple drawings or writing things down are concrete things that patients can relate to and hold on to even when they leave. During fellowship, one of my attendings would enter every new patient consult with a legal pad. He would write out in bullet points the summary of the patient’s visit and treatment options, and then hand them to the patient. He would ask them to email him with any questions after the visit. He would often joke that he would judge his teaching of the patients by how few emails he received. This is a skill that comes with practice and requires adapting to each individual patient and situation.
I knew I had to do my best to teach the patient sitting in front of me. On his laptop he had a sticker of Pac-Man. I used that as inspiration and we started talking about Pac-Man and T cells. Yes, it sounds a little odd now, but the words just kept flowing.
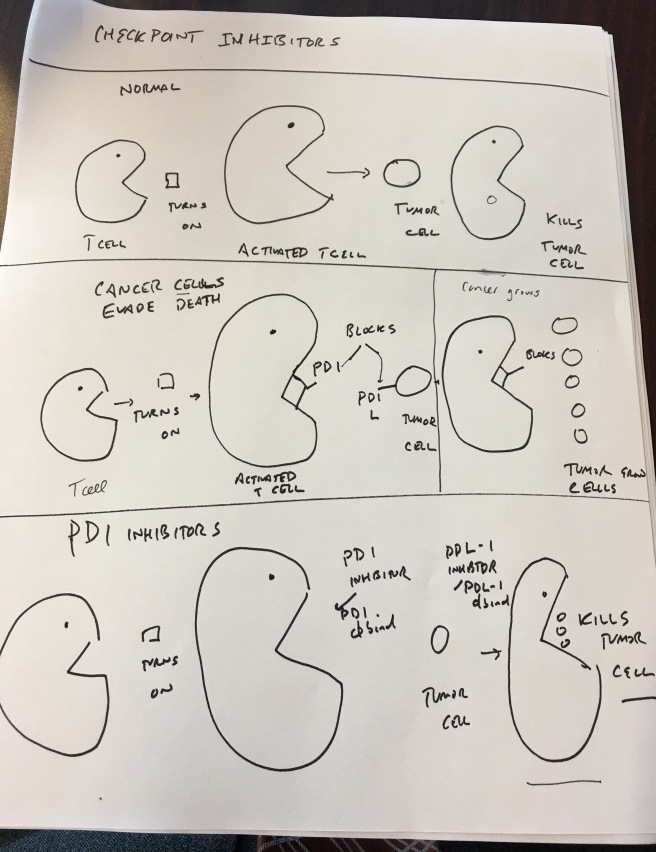
I explained how our body was pre-wired to kill cancer cells by using activated T cells. These T cells are sometimes kept in check by certain proteins expressed on the T cells or tumors. These tumors can evade these T cells by expressing checkpoints that make the T cells ineffective and unable to effectively kill cancer cells. A new class of drugs called checkpoint inhibitors can actually block these proteins that are expressed on tumor and T cells and, in essence, cause T cells to then kill cancer cells.
He interrupted, “But what about Pac-Man?”
I said, “Think of Pac-Man as the T cells eating up the dots, which are like the cancer cells. Checkpoints are expressed and can put a clamp on Pac-Man and not let him eat the dots. Yet using these new checkpoint inhibitors, we can block the clamp and reactivate Pac-Man to eat the dots, effectively destroying tumor cells.” This analogy framed the long talk about the ups and downs of this therapy and the potential it could bring.
The patient left the hospital and improved. We started him on therapy and, like Pac-Man, his T cells started to eat up those tumor cells. He has had a dramatic response and has a newfound hope and optimism about his future. The patient remembered the Pac-Man talk and made a drawing that he gave me to me. This drawing has served as an example to help many of my future patients understand checkpoint inhibitors. (I've shared it at the bottom of this post, in case you want to show it to your own patients when explaining T cells and checkpoint inhibitors.)
We have a long road ahead to curing cancer, yet the promise of new drugs and treatments is what motivates me as an oncologist. My experience with this patient taught me a huge lesson about our role as doctors. Whether we realize it or not, whether we work in an academic center or not, we are teachers when it comes to our patients.
I challenge you to remember this when you are explaining a procedure to a patient or getting informed consent. Take the time to teach them and find a way to reach the patient so they can be a partner in the journey. Being an effective patient educator enables doctors to gain the trust of our patients and help gain their cooperation in following our future recommendations.
Originally published on Cancer Doc in Evolution; reprinted with permission.

Recent posts