Jan 06, 2011
by Elyse Blye, Editorial Assistant
With registration open for Stage 1 of the Center for Medicare and Medicaid Services’ (CMS) Electronic Health Records (EHR ) Incentive Program, 2011 will be the year for oncologists to evaluate the practice changes they need to make in order to move to EHRs, select a product that best fits their budget and clinical needs, and understand what their obligations are in order to qualify.
Addressing a “rapidly changing health care environment”
The paper medical record is a tool primarily designed to be seen and used by an individual physician. Often, it is organized as the individual desires, using whatever shorthand method of charting works best with the least expenditure of time and effort. This antiquated approach makes it extremely difficult, if not impossible, for oncologists to practice medicine in the most efficient, effective, and safest way possible.
“While it does allow maximum use of office time for face-to-face physician/patient encounters,” said ASCO Health Information Technology (HIT) Work Group Chair Peter Yu, MD, of Palo Alto Medical Foundation, “the recordkeeping does not support anyone else using the chart. One has only to think about the last time they saw a new patient who was transferring care from another physician and brought in a five-inch exploding paper chart for you to review.”
On the contrary, EHRs:
- allow for interoperability—giving other health care professionals, beyond the primary recorder of information, access to patient information
- reduce paperwork
- support the delivery of standardized care
- improve patient safety, especially by means of embedded clinical decision support
- ensure that clinical and demographic information is available when, where, and how the user wants it
|
“All EHRs have at least three layers: the top layer supports data input, the bottom layer is your underlying database of information, and the middle layer connects the dots between the content you input and store in the database,” according to ASCO’s 2008 handbook, Oncology Electronic Health Record Field Guide: Selecting and Implementing an EHR.
“Yes, it takes a lot more time to do this—time that is taken away from patient time or from physician time— but I would argue that in the past, we were skimping on documentation and just not doing a high-quality job in an area that directly impacts patient care,” Dr. Yu said. “EHRs are a necessary tool to adopt and to adapt to a rapidly changing health care environment.”
Understanding the incentive program
The EHR Incentive Program falls under the Health Information Technology for Economic and Clinical Health (HITECH) Act, which is a part of the American Recovery and Reinvestment Act (ARRA) of 2009. CMS worked with the Office of the National Coordinator (ONC) for Health Information Technology in developing standards, implementation specifications, and certification criteria for EHR technology.
Under the program, the phrase “meaningful use” is described as using certified EHR technology to improve quality, safety, efficiency, and to reduce health disparities. The technology must be used in such a way that engages patients and families in their health care, improves care coordination, and improves public health, all while maintaining privacy and security.
Medicare incentives for eligible professionals
Medicare incentives for eligible professionals are capped at $44,000 per professional. This amount is the maximum, aggregate amount of incentive payment. One must demonstrate “meaningful use” every year for five years to receive the total payment, though it is possible to qualify for less.
The incentive program does not extend indefinitely. As it ends in 2016, one can only receive a maximum payment by participating in the program from 2011 to 2015. The last day for eligible professionals to register and attest to receive an incentive payment for calendar year 2011 is February 29, 2012.
Medicaid incentives for eligible professionals
The Medicaid incentive program is separately managed by each state. However, the maximum aggregate incentive payment is $63,750. Eligible professionals can qualify for payments as late as 2016.
Medicare and Medicaid incentives for hospitals
The incentives for hospitals are slightly more complicated, as the incentive amount for each year is based on a number of factors. However, they begin with a $2 million base payment. Incentive payments for hospitals are based on the federal fiscal year (October 1– September 30 of the following year).
Stage 1 of the incentive program sets the baseline for electronic data capture and information sharing (see text box). Stage 2 (est. 2013) and Stage 3 (est. 2015) will continue to expand on this baseline and be developed through future rule making.
 |
|
|
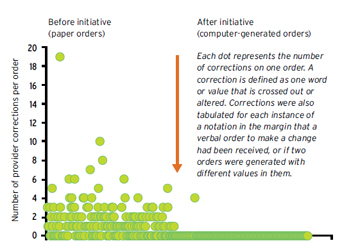
Figure 1: Impact of Software on Providers’ Corrections to Chemotherapy Orders
|
Details of the EHR Incentive Program—including eligibility information, timelines, and maximum incentive payment amounts—can be found at asco.org/ehr and cms.gov/EHRIncentivePrograms.
An EHR success story
Anna E. Schorer, MD, of VA Midwest Health Care Network and an ASCO HIT Work Group member, is a strong proponent of EHR adoption and has a proven track record of successfully implementing their use. In November 2010, Dr. Schorer and her team received a Network Star Award for “the spread of strong practice” through their implementation of oncology EHRs at VA sites in a five-state region.
Before implementing an EHR system, the VA sites evaluated problems they had previously encountered using a non-electronic system for chemotherapy orders. “There were many kinds of errors—most of which tended to be on the physician side,” Dr. Schorer noted.
These pre-EHR errors included:
- dose miscalculation
- incorrect rule insertion
- omissions—Dr. Schorer noted this as one of the most prevalent of all errors, in which individual components to an order were omitted by the physician (including supportive medications, hydration, lab monitoring, etc.)
- timing, such as misstating when a treatment was meant to start, or not including that information at all
- patient identification
 |
|
|
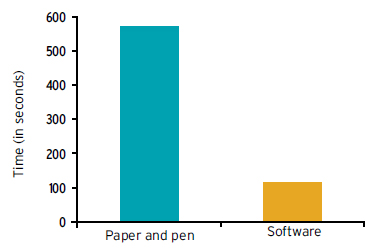
Figure 2: Time Needed for Providers to Write Chemotherapy Orders
|
Errors relating to transcription in administration were also noted on the nursing and pharmacy side. Many of the errors could be traced back to the original problem—a physician omitting details or writing something that was unclear, ambiguous, or illegible.
Prior to her team’s EHR implementation, patient orders frequently required one or more physician revisions, according to Dr. Schorer. But once EHRs were in place, physician corrections were significantly reduced (see Figure 1). Furthermore, it took an average of 10 minutes to write out a complicated chemotherapy order set prior to EHRs, but once in place, time was significantly reduced, averaging less than three minutes (see Figure 2).
Making the transition
Transition from paper to EHRs is not easy and must be undertaken with patience and involvement at all staff levels, explained ASCO HIT Work Group member Lawrence Shulman, MD, of Dana-Farber Cancer Institute: “Practices should understand that there is a significant amount of inefficiency associated with the introduction of an EHR , but with time, most oncology groups find that their practice is much more efficient and safe with an EHR than with paper records,” he noted.
From a decision-making standpoint, ASCO HIT Work Group member Scott M. Herbert, MD, of New Mexico Cancer Care, suggests that administrators and physicians implement EHRs in a “spirit of connectivity,” taking into consideration the product type and the needs of the community in which the practice resides. “I would like to see ASCO be more involved helping practices analyze their markets, the other physician groups and hospitals in the markets, and finding systems that are truly integrative, rather than very extensive data silos,” he explained.
Future possibilities
To facilitate translation from trial design to the bedside, Dr. Schorer envisions ASCO developing and encouraging standardized vocabulary for the oncology community around each potential component of a chemotherapy order set. From that concept, all data presented throughout the oncology field, including what is published in the Journal of Clinical Oncology, would be uploaded onto a website or in a database, allowing for the exchange of knowledge between all oncology facilities.
| ASCO at the Helm: Promoting EHR Use To help address the challenges of a transition, ASCO has sponsored an EHR Lab at the Annual Meeting since 2007 and will continue to do so at this year’s Meeting. ASCO also held EHR symposia for members and the EHR vendor community in 2007 and 2009; the 2011 EHR symposium will take place this fall. In addition, ASCO members are well represented on the Certification Commission for Health Information Technology (CCHIT ) work group, which develops certification criteria for oncology EHRs. |
Share your thoughts on EHRs and usability on the ASCO Connection forums.
